In the first post of this series, we looked at nursing home census as a measure of the financial health of a facility like DeKalb County Rehab & Nursing (DCRNC). In fact, DCRNC gave great census, its occupancy mostly in the 170s and even 180s from 2015 until 2019. Consistently high census numbers kept revenues aloft and the expense side easy to ignore at first.
One answer is staffing
Turnover of staff in nursing homes is not news, but DCRNC’s experiences are unusual, involving losses on a scale that undoubtedly can erode performance and cohesion. Staff retention issues began worsening for management beginning 2016 and, as they continued, became striking in comparison to the years preceding. Including interim and acting administrators, six people have occupied the administrator role since 2015 (four of them since 2018). Positions of director of nursing, assistant director of nursing, social services director, dietary director, business office manager, and compliance officer have also turned over during this period, most of them multiple times.
Using operating board meeting minutes, I counted 17 management departures — but of course there’s no guarantee all of them were announced and recorded.
As management struggled, nursing staff became the next domino. DCRNC could not achieve traction in retention. The state mandates minimum staffing requirements for nurses and CNAs, and to my knowledge, DCRNC has always made its minimums. But they’ve done it by using temporary nurses provided by outside agencies (aka registries). DCRNC has become increasingly dependent on agency staff and these temporary nurses are more expensive, earning perhaps as much as 25% to 40% more than in-house personnel.
Staff revealed during an operations board meeting in November 2019 that 60% of the CNAs working at DCRNC at that time were agency. That’s not just an operating loss, it’s a hemorrhage, as shown below.
Another answer is budgeting
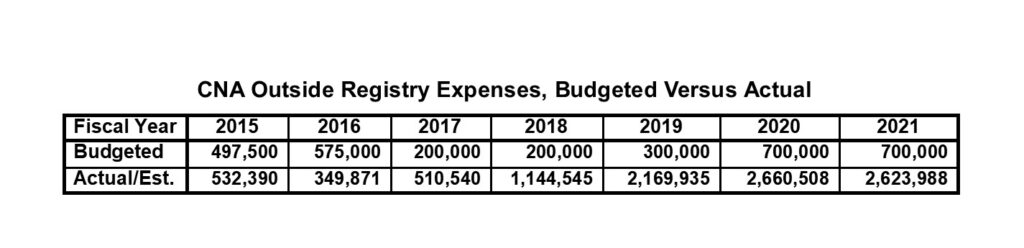
See? Hemorrhage.
RN and LPN registry expenses saw similar patterns of steep increases, but there are fewer of the nurses so the budget deficits haven’t reached the drama of single-year, million-dollar deficits as the CNA expenses have.
As I understand it, the annual DCRNC budget goes through three layers of scrutiny: The DCRNC Operating Board, the Health & Human Services Committee of the DeKalb County Board, and the County Board itself. I wonder if any of them asked how DCRNC was planning to reduce 2018’s $1.1 million CNA agency staffing expense by $800,000 in one year. If they did ask, I suppose the DCRNC budgeteers might have explained that the leadership had changed and all would be well, not understanding that a crisis several years in the making might require a bit more time, sweat, and care.
In our third article in this series, we’ll have a look at the budgeteers.
[wpedon id=3817]